Image credit: Scott Bauer, US Government, Public Domain


From a contaminated dish in London to saving lives on the D-Day beaches of Normandy (via dedicated scientists in Oxford and Peoria), pencillin has saved many millions of lives.
“When I woke up just after dawn on September 28, 1928, I certainly didn’t plan to revolutionize all medicine by discovering the world’s first antibiotic, or bacteria killer. But I guess that was exactly what I did.”
Alexander Fleming
There are many things we take for granted these days that were discovered entirely by accident; X-rays, the microwave, and Play-Doh, to name just a few. One of the most famous cases of a revolutionary discovery made unexpectedly is penicillin, the first antibiotic. Before antibiotics, even the most innocuous of cuts could be fatal; but that changed with the work of Alexander Fleming, Ernst Chain and Howard Florey.
Post-holiday clean up
Professor of Bacteriology Alexander Fleming returned from a holiday in September 1928 to notice mouldy contamination on one of his many petri dishes of Staphylococcus bacteria.
The zone surrounding the mould was clear of bacteria, suggesting to Fleming that something about this mould was deadly. He identified the mould as a strain of Penicillium notatum, and decided to name the active component “penicillin”. He tried to grow several other moulds to see if they had the same effect on the Staphylococcus, but only the P. notatum was able to kill the bacteria.
Though Fleming is the most famous person in the story of the discovery of penicillin, he was unable to purify it. He ended his studies into it in 1931, and agreed to send the mould to anyone wishing to isolate penicillin. Ernst Chain, of Oxford University, was one such person.
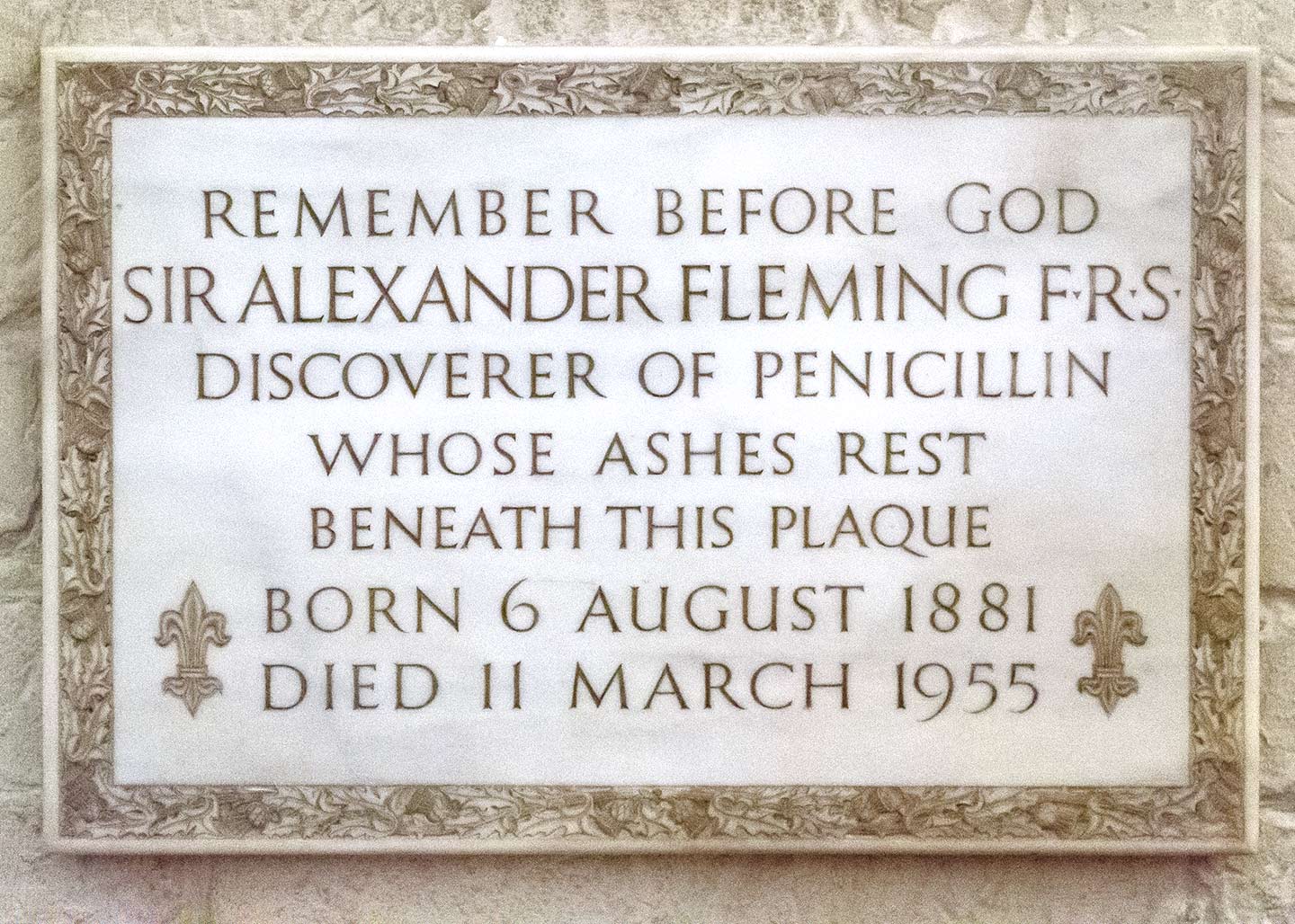
Alexander_Fleming_Plaque_1440
Image Credit: Photo by CEphoto, Uwe Aranas
Oxford joins the mission
In 1939, Chain worked with his supervisor, Howard Florey, and fungal expert Norman Heatley. They were able to describe the conditions in which the Penicillium mould best grows, and devised a way to isolate penicillin. They found it to be a powerful killer of bacterial infections in mice, with minimal side effects.
The first person to be given penicillin was Albert Alexander in 1940, who was dying from an infection that left him with abscesses in his lungs, and on his eyes and face. He developed the infection after scratching himself while pruning roses. Alexander was injected with penicillin, and within a couple of days made a remarkable improvement, but as the supply of available penicillin was too small to fully treat his infection, he died soon after.
Press attention
By the early 1940s, penicillin was seen as a miracle cure, and Sir Almroth Wright – Alexander Fleming’s boss – wrote to The Times to ensure they knew of Fleming’s contribution. While Fleming went on to discuss penicillin with the press, Howard Florey disliked publicity and refused to. He also prevented the rest of the Oxford University researchers from speaking to newspapers. Thus began the popular belief that Fleming was the only person involved in the discovery of penicillin.
Melons and mass production

raspberry_melon_mould_1440
Image Credit: AdobeStock
Once penicillin had been isolated, the problem of producing the drug on a mass scale remained. 2,000 litres of P. notatum mould culture fluid were needed to produce enough pure penicillin to treat blood poisoning in a single person. It then fell to American drug companies to mass produce penicillin, in time for the USA entering the Second World War. The search for a fungus that would produce more penicillin per litre began.
In another flash of serendipity, Mary Hunt, a laboratory assistant at the US Northern Regional Research Laboratory, came across a cantaloupe melon with a golden mould. This mould turned out to be P. chrysogenum, and yielded 1,000 times more penicillin than Alexander Fleming’s P. notatum.
In 1949, Florey noted “had it not been for [the US drug companies’] efforts there would certainly not have been sufficient penicillin by D-Day in Normandy in 1944 to treat all severe casualties, both British and American”.
Awards season
Dorothy Hodgkin used X-ray crystallography to determine the chemical structure of penicillin in 1945. In that same year, Alexander Fleming, Ernst Chain and Howard Florey were awarded the Nobel Prize in Medicine for their work.
In his Nobel Banquet speech, Fleming himself commented on how often “fortune intervened” in the discovery of penicillin. If not for the accidental contamination of his culture plate, the outbreak of war that allowed for large-scale production of medicines, and Mary Hunt happening upon the right cantaloupe, we might not have the medical miracle we so take for granted today.
Future prospects
Another warning that Fleming gave back in 1945 was to not abuse antibiotics, as signs of antibiotic resistance in bacteria were already beginning to show. Today antibiotic resistance is a dangerous threat. Nicole Wheeler, a data scientist at the Sanger Institute, said, “A 2014 UK government review estimated that by 2050 10 million deaths will occur due to antimicrobial-resistant infections. What’s really scary about this figure is the fact this estimate doesn’t take into account what an integral part of modern healthcare antibiotics have become. Antibiotics haven’t just given us the ability to treat infections, they’ve also underpinned fundamental changes in modern medicine. Without antibiotics routine surgery, caesarean sections, chemotherapy would all be incredibly risky procedures. With growing resistance, some medical procedures we’ve come to take for granted may become more trouble than they’re worth.”
Nicole is part of the Centre for Genomic Pathogen Surveillance, which is helping the fight against high-risk disease-causing bacteria, with a focus on antibiotic resistance. The centre partners with others across the world to get a better understanding of how antibiotic resistance emerges and spreads. By identifying high-risk strains and the spread of antibiotic resistant bacteria as soon as possible, efforts can be focused to eliminate resistance as it appears.
We can’t rely on fortune to intervene again.






